Knee arthritis can lead to difficulty in doing many everyday activities, such as walking, climbing stairs or sitting cross legged. It is one of the major causes of lost work time and serious disability for many people.
There are more than 100 different forms of arthritis, of which the most common types are osteoarthritis and rheumatoid arthritis. While arthritis is mainly a disease of adults and elderly, some forms can affect children also.
Although arthritis is irreversible, there are many treatment options available to help manage pain and let people stay active.
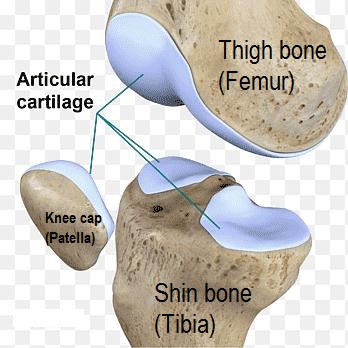
Anatomy of the knee joint
The knee is the largest and strongest joint in your body. It is made up of the lower end of the femur (thighbone), the upper end of the tibia (shinbone), and the patella (kneecap). The ends of the three bones where they touch are covered with “articular cartilage” (hyaline cartilage) , a smooth, 2-4 mm sized yellowish slippery substance that protects and cushions the bones as you bend and straighten your knee.
Two wedge-shaped pieces of cartilage are called “meniscus” which act as "shock absorbers" between your thighbone and shinbone. They are tough and rubbery to help cushion the joint and keep it stable.
The knee joint is surrounded by a thin lining called the synovial membrane. This membrane releases a fluid that lubricates the cartilage and reduces friction.
Major types of arthritis affecting knee
The major types of arthritis that affect the knee are osteoarthritis, rheumatoid arthritis, and post-traumatic arthritis.
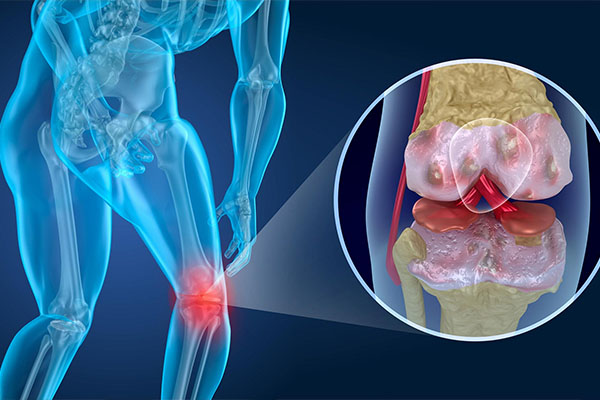
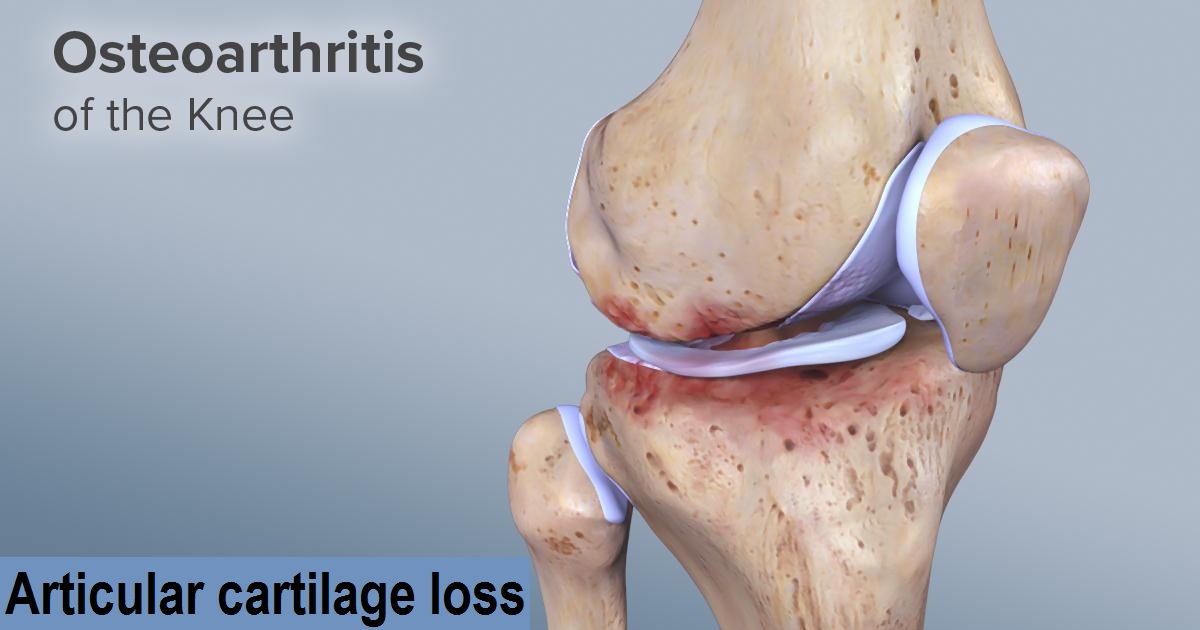
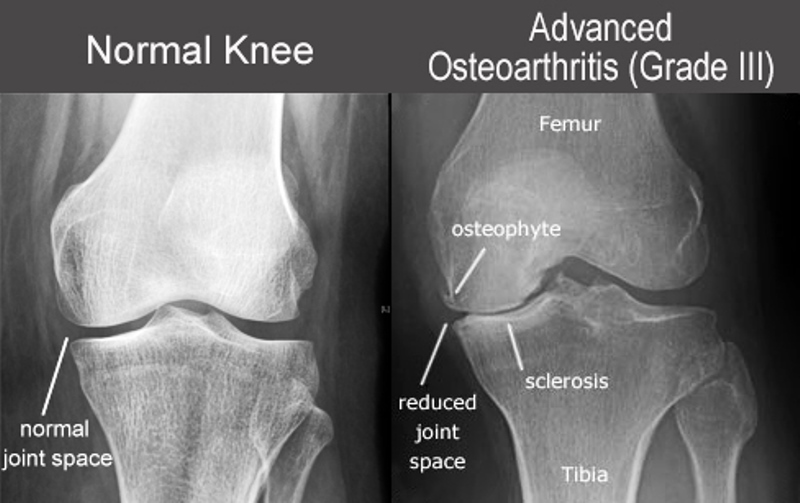
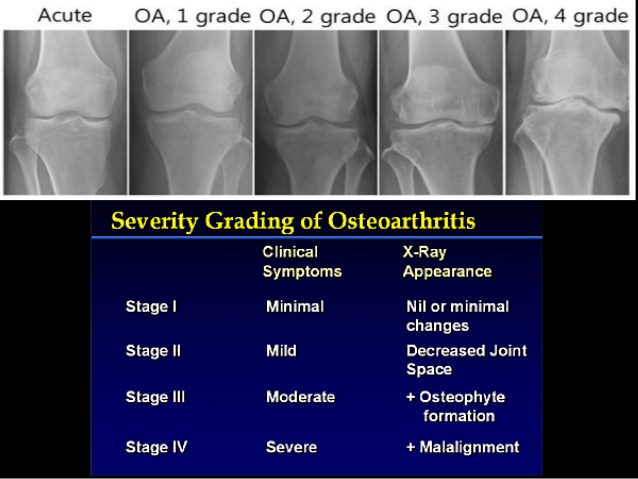
(1) Osteoarthritis : Osteoarthritis is the most common form of arthritis in the knee. It is a degenerative,” wear-and-tear" type of arthritis that occurs most often in people 50 years of age and older, but may occur in younger people, too. In osteoarthritis, the cartilage in the knee joint gradually wears away. As the cartilage wears away, it becomes frayed and rough, and the protective space between the bones decreases. This can result in friction between bones during movement, and produce painful bone spurs.
Osteoarthritis is typically a slow progressive disease that may eventually lead to disability. The intensity of the clinical symptoms may vary on individual basis. However, they typically become more severe, more frequent, and debilitating over time. The rate of progression also varies for each individual.
Main causes for developing Osteoarthritis of knee are
- Post-traumatic
- Post-surgical
- bruising
- Congenital malformation of the limb
- Mal-alignment of the knee (varus/valgus)
- Scoliosis
- Rickets
- Hemochromatosis
- Chondrocalcinosis
- Ochronosis
- Wilson disease
- Gout
- Pseudogout
- Acromegaly
- Avascular necrosis
- Rheumatoid arthritis
- Infectious arthritis
- Psoriatic arthritis
- Hemophilia
- Paget disease
Risk Factors for Knee OA - Modifiable
- Weight / obesity
- Occupation – prolonged standing and repetitive knee bending,
- Contact sports (e.g. Tennis , Football)
- Muscle weakness or imbalance (e.g.Quadriceps weakness)
- Health – metabolic syndrome
- Articular trauma to the knee joint
Risk Factors for Knee OA-Non Modifiable
- Gender - females more common than males
- Old age
- Genetics
- Race
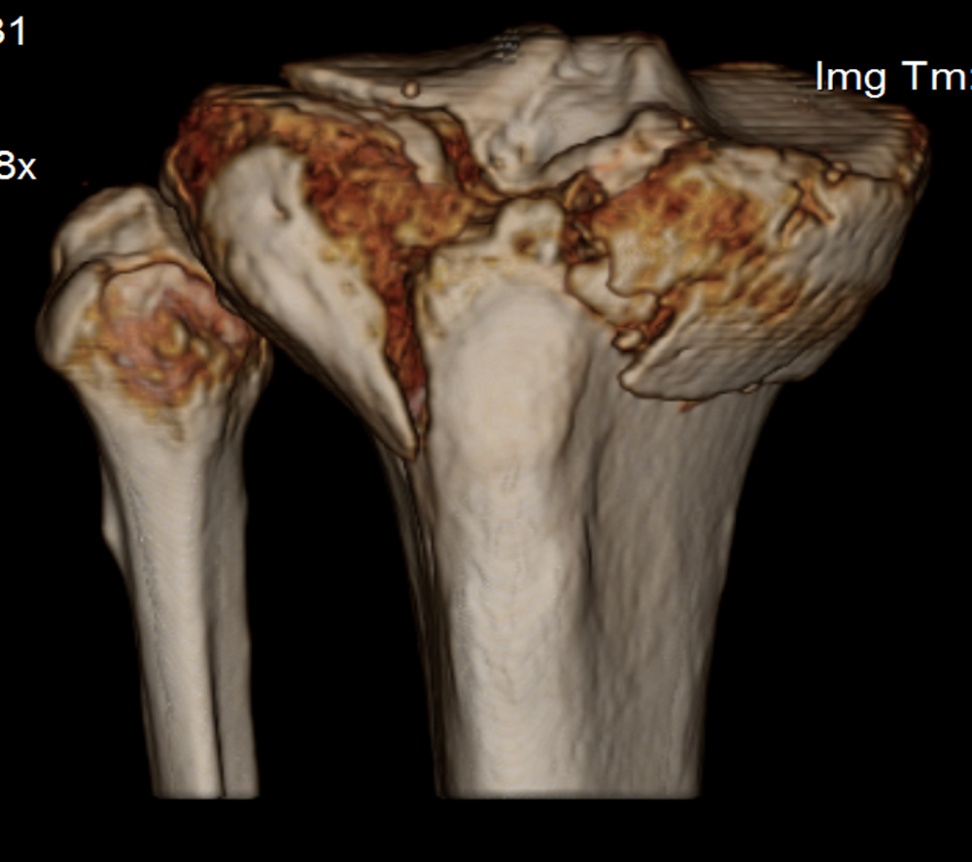
CARTILAGE LOSS AT FEMUR & TIBIA
VARUS DEFORMITY OF KNEE
(2) Rheumatoid Arthritis : Rheumatoid arthritis is a chronic disease that attacks multiple joints throughout the body, including the knee joint. It is symmetrical, that means it usually affects the same joint on both sides of the body. In rheumatoid arthritis the synovial membrane that covers the knee joint begins to swell, and this results in knee pain and stiffness.
Rheumatoid arthritis is an autoimmune disease. This means that the immune system attacks its own tissues. The immune system damages normal tissue such as cartilage and ligaments and softens the bone.


VALGUS DEFORMITY OF KNEE AND REDUCTION IN LATERAL COMPARTMENT OF KNEE


(3)Post-traumatic Arthritis Posttraumatic arthritis is form of arthritis that develops after an injury to the knee. For example, a broken bone may damage the joint surface and lead to arthritis years after the injury. Meniscal tears and ligament injuries can cause instability and additional wear and tear of the knee joint, which over time can result in osteoarthritis of knee.
Epidemiology
Knee osteoarthritis is the most common type of arthritis diagnosed, and its prevalence will continue to increase as life expectancy and obesity rises. Depending on the source, roughly 13% of women and 10% of men 60 years and older have symptomatic knee osteoarthritis. Among those older than 70 years of age, the prevalence rises to as high as 40%. The prevalence of knee osteoarthritis in males is also lower than in females. Interestingly, not everyone who demonstrates radiographic findings of knee osteoarthritis will be symptomatic. The incidence of symptomatic knee osteoarthritis is roughly 240 cases per 100,000 people per year
Symptoms
A knee joint affected by arthritis may be painful and inflamed. Generally, the pain develops gradually over time, although sudden onset is also possible. There are other symptoms, as well:
- The joint may become stiff and swollen, making it difficult to bend and straighten the knee.
- Pain and swelling may be worse in the morning, or after sitting or resting.
- You may have difficulty in sitting cross legged, squatting, climbing / descending the stairs.
- There may be a localised swelling / cyst formation in the back of your knee
- Vigorous activity may cause pain & swelling to flare up.
- Loose fragments of cartilage and other tissue can interfere with the smooth motion of joints. The knee may "lock" or "get stuck" during movement. It may creak, click, snap or make a grinding noise (crepitus).
- Pain may cause a feeling of weakness or buckling in the knee.
- There might be bowing deformity of your knee / lower limb & associated limp while walking along with decreased walking capacity.
- Many people with arthritis note increased joint pain with cold / rainy weather.
- Any signs of injury to the muscles, tendons, and ligaments surrounding the knee
Knee Pain And difficulty in stair climbing


Examination by Doctor
During your appointment, Doctor will ask you about your symptoms and medical history, conduct a physical examination, and possibly order diagnostic tests, such as x-rays or blood tests and rarely MRI also.
Physical Examination

During the physical examination, Doctor will look for:
- Joint swelling, warmth, or redness
- Tenderness about the knee
- Range of passive (assisted) and active (self-directed) motion
- Instability of the joint
- Crepitus (a grating sensation inside the joint) with movement
- Pain when weight is placed on the knee
- Instability of the joint
- Problems with your gait (the way you walk)
- Power of muscles around knee joint
- Any signs of injury to the muscles, tendons, and ligaments surrounding the knee
- Involvement of other joints (like in rheumatoid arthritis)
- Involvement of other joints (like in rheumatoid arthritis)
EFFUSION

Imaging Tests
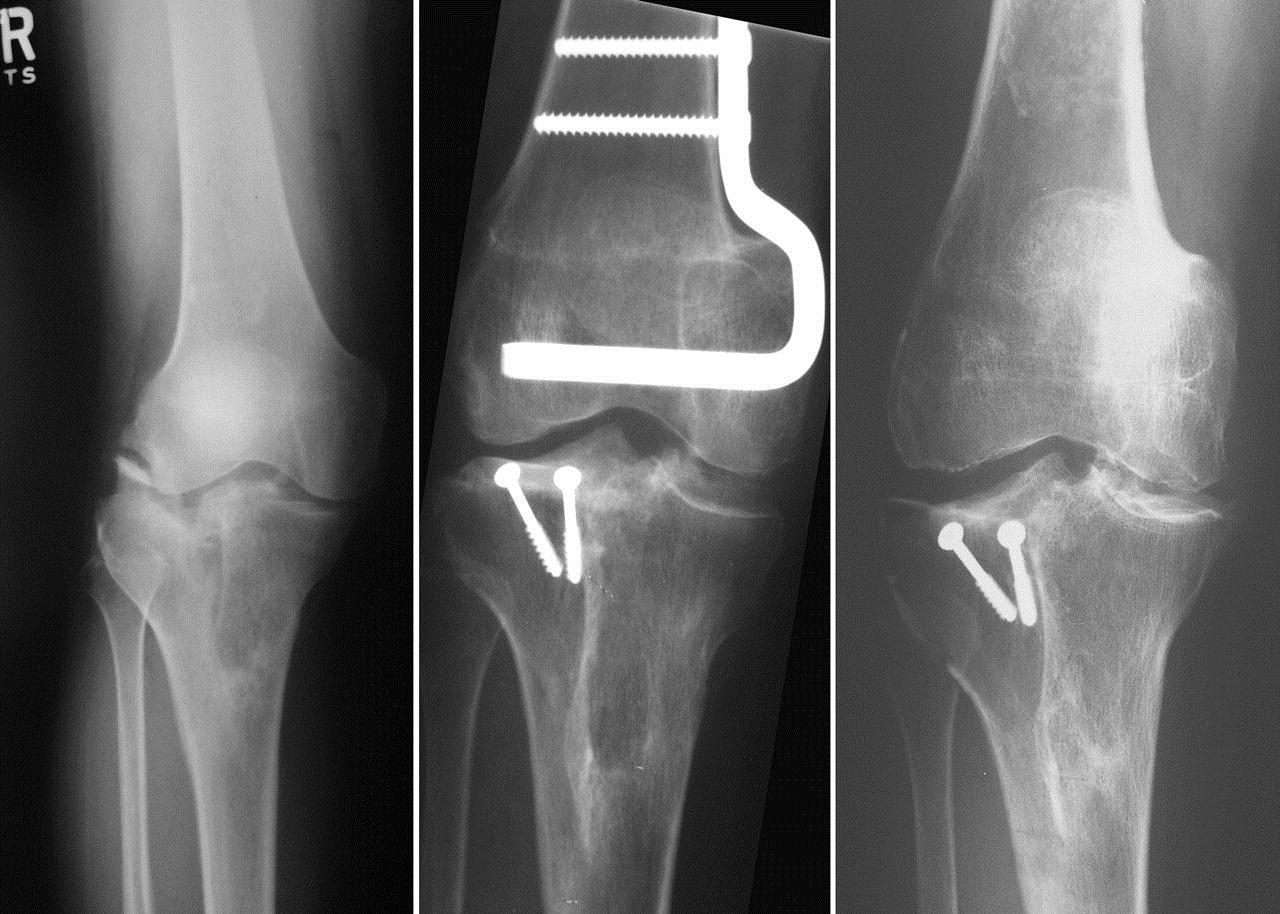
X-rays.- Knee – AP(standing) / Lateral / Skyline views These imaging tests create detailed pictures of dense structures, like bones. They can help distinguish among various forms of arthritis. The plain radiograph serves as the primary investigation in the diagnosis of knee OA, as well as in assessing the severity of the disease. X-rays of an arthritic knee may show a narrowing of the joint space, the formation of bone spurs (osteophytes), changes in the bone like subchondral bone sclerosis & cyst formation, osteochondral bodies and bone deformities.
Treatment
There is no cure for arthritis but there are a number of treatments that may help relieve the pain and disability it can cause.
(A)Nonsurgical Treatment
As with other arthritic conditions, initial treatment of arthritis of the knee is nonsurgical. Doctor may recommend a range of treatment options.
1.Lifestyle modificationsSome changes in your daily life can protect your knee joint and slow the progress of arthritis.
- Minimize activities that aggravate the condition, such as climbing stairs.
- Switching from high impact activities (like jogging or tennis) to lower impact activities (like swimming or cycling) will put less stress on your knee.
- Losing weight, if you are obese , can reduce stress on the knee joint, resulting in less pain and increased function.
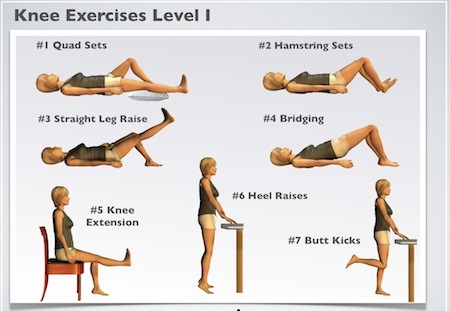
2. Physical therapy Lower limb musculature is the natural brace for the knee joint. Quadriceps strength deficits have been reported in 20%–70% of patients with knee OA. Specific exercises can help increase range of motion and flexibility, as well as help strengthen the muscles in your leg. Your doctor or a physical therapist can help develop an individualized exercise program that meets your needs and lifestyle.
3. Assistive devices Using devices such as a cane, wearing shock-absorbing shoes or inserts, or wearing a brace or knee sleeve can be helpful. A brace assists with stability and function, and may be especially helpful if the arthritis is centred on one side of the knee. There are two types of braces that are often used for knee arthritis: An "unloader" brace shifts weight away from the affected portion of the knee, while a "support" brace helps support the entire knee load.


(B)Surgical Treatment
Doctor may recommend surgery if your pain from arthritis causes disability and is not relieved with nonsurgical treatment. As with all surgeries, there are some risks and possible complications with different knee procedures. Your doctor will discuss the possible complications with you before your operation.
1. Arthroscopy This treatment applies mostly to the knee. It is only considered in certain situations as it will not be effective in most patients. Hip arthroscopy is difficult and not recommended for moderate to advanced arthritis. This procedure is done as a day care surgery and involves two or three small incisions over the knee. A camera is inserted into the joint and the joint surfaces and shock absorber cartilage (meniscus) are inspected. Any loose bits of cartilage are flushed out and meniscal tears are also trimmed. This procedure works best with early osteoarthritis and is not recommended for advanced cases. The success rate in the literature is about 60%, although symptoms can return after 1-2 years. There is a low risk of infection (1 in 100 or less), and stiffness can occasionally be a problem. Blood clots in the leg after surgery are extremely rare. The occasional patient may have more knee pain after an arthroscopy so each patient must consider the risks and the benefits of the procedure. Recovery following surgery usually between 3-6 weeks, but occasionally can take longer depending on the patient and their knee.

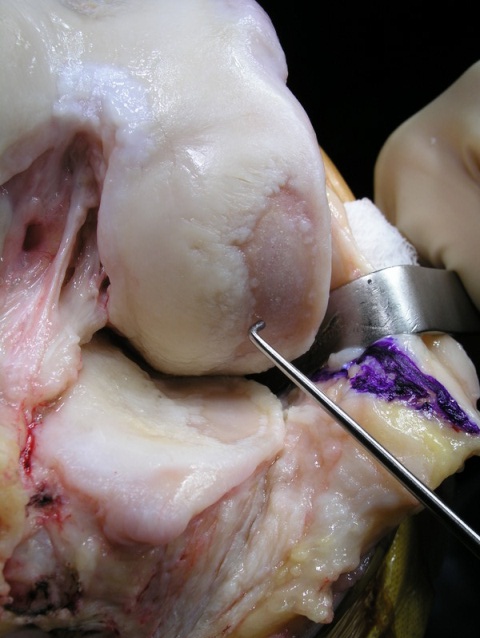
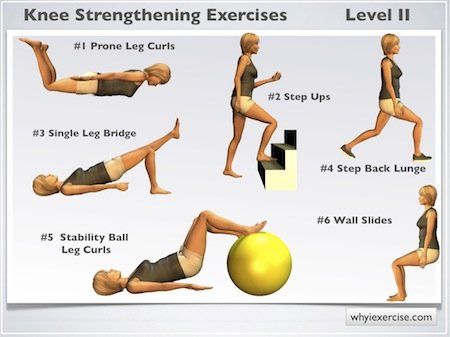
2. Cartilage grafting Normal, healthy cartilage tissue may be taken from another part of the knee or from a tissue bank to fill a hole in the articular cartilage. This procedure is typically considered only for younger patients who have small areas of cartilage damage.
3. Synovectomy The joint lining damaged by rheumatoid arthritis is removed to reduce pain and swelling.

4. High tibial osteotomy- This procedure may be appropriate for a younger patient (less than 50 yrs) without significant leg malalignment and only one part of the joint affected (either the inside or the outside). It involves making a cut in the tibia bone and re-aligning the limb to take pressure off of the arthritic part of the knee. By shifting your weight off the damaged side of the joint, an osteotomy can relieve pain and significantly improve function in your arthritic knee. In the properly selected patient, this procedure can work well for up to 10 years. The advantage is that once the bone heals, a patient can run, jump or do whatever they want on the knee without worrying about ruining a partial or complete joint replacement. Osteotomies are not typically done for hip arthritis except in rare cases.



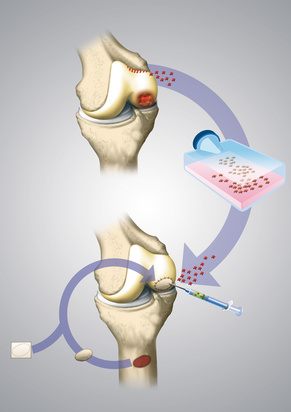
5. Uni-compartamental knee arthroplasty / Microplasty - This is essentially a partial knee replacement of either the inside or the outside portion of the knee. It can rarely be done for arthritis of the knee cap in select patients. This procedure is best suited for low to moderate demand patients who are slim with good range of motion of the knee. The operation itself is done through a smaller incision and results in less pain, less blood loss and a shorter hospital stay compared to a total knee replacement. Patients have a more normal feeling knee as most of the joint remains intact. The long term survival of these implants at 10 years is greater than 90%, making them an attractive option in the appropriately selected patient. Only your surgeon can decide whether you are a candidate for this operation or not.
6. Total knee replacement (TKR) Doctor will remove the damaged cartilage and bone, and then position new metal or plastic joint surfaces to restore the function of your knee. Here, one exception is the patella (kneecap). If this is very healthy at the time of the surgery, it will be left alone and not resurfaced. Leaving a healthy patella alone does not affect the results of the surgery in terms of pain relief. Knee replacement surgery is highly successful (>95%) at relieving pain. The recovery and rehabilitation is a little bit harder than a total hip replacement. Most patients require a full 1 to 3 months to recover motion and strength in the leg. Patients must work very hard to get good knee bending after surgery or it may not flex an adequate amount. Rarely, a patient will require a manipulation under anaesthesia to achieve proper motion, in the case of knee stiffness.

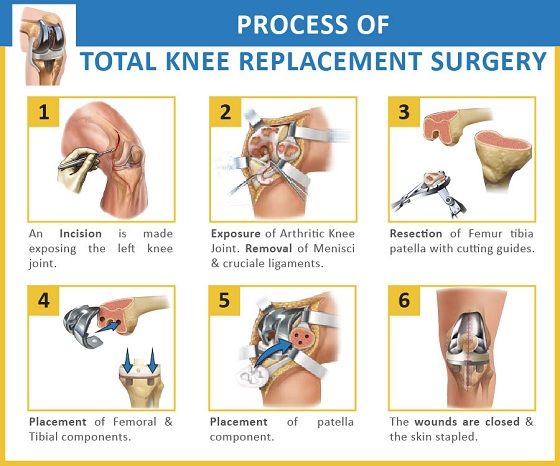
TKR Surgery Procedure Information
The knee is an important hinge joint and as it is weight-bearing can be prone to “wearing out”. Arthritis is painful and disabling and you and your surgeon may have decided that a knee replacement may be your best option
A knee replacement is a surgical procedure, in which the injured or damaged running surfaces of the knee are replaced with artificial parts which are secured to the bone.
You will be seen by the surgeon before the operation. They will take this opportunity to draw (mark with a pen) on your leg. This is to make sure the correct leg is operated on. If you have any questions, this might be a good time to ask them.
An anaesthetic will be administered in theatre. This may be a general anaesthetic (where you will be asleep) or a regional / local block (e.g. where you are awake but the area to be operated is completely numbed). You must discuss this with the anaesthetist.
A tight inflatable band (a tourniquet) may be placed across the top of the thigh to limit the bleeding. Your skin will be cleaned with anti-septic solution and covered with clean towels (drapes). The surgeon will make an incision (a cut) down the middle of the knee. The knee capsule (the tough, gristle-like tissue around the knee) which is then visible can be cut and the knee cap (patella) pushed to one side. From here, the surgeon can trim the ends of the thigh bone (femur) and leg bone (tibia) using a special bone saw. Some surgeons also remove the underside of the knee cap, if required.
Using measuring devices, the new artificial knee joints are fitted into position. The implants have an outer alloy metal casing with a “polyethylene” bearing which sits on the tibia. A polyethylene button is sometimes placed on the underside of the knee cap. When the surgeon is happy with the position, fixation and movements of the knee, the tissue and skin can be closed. This may be done with stitches (sutures) or metal clips (skin staples). The clips and stitches will need to be removed around 10 – 20 days after the operation, once the skin heals well.
Drains may be used, and if so can be pulled out easily in the ward after a day or two. When you wake up, you will have a padded bandage around the knee. If you are in pain, please ask for pain killers. If you have pain, it is important that you tell somebody. You will go for an X-ray the on same day or day after the operation and will be encouraged to stand and take a few steps from same day evening or next day.
You will be visited by the doctor / physiotherapy team, who will suggest exercises for you. It is important to do these (as pain allows).
Meet Our Doctors

Dr. Nitin Thakkar
M.S (Ortho)

Dr. Shweta Thakkar
DMRD, DNB (Radio-Diagnosis)