Osteoarthritis of the hip causes pain and stiffness. It can make it hard to do everyday activities like bending over to tie a shoe, rising from a chair, or taking a short walk. Because osteoarthritis gradually worsens over time, the sooner you start treatment, the more likely it is that you can lessen its impact on your life. Although there is no cure for osteoarthritis, there are many treatment options to help you manage pain and stay active.
Anatomy of the knee joint
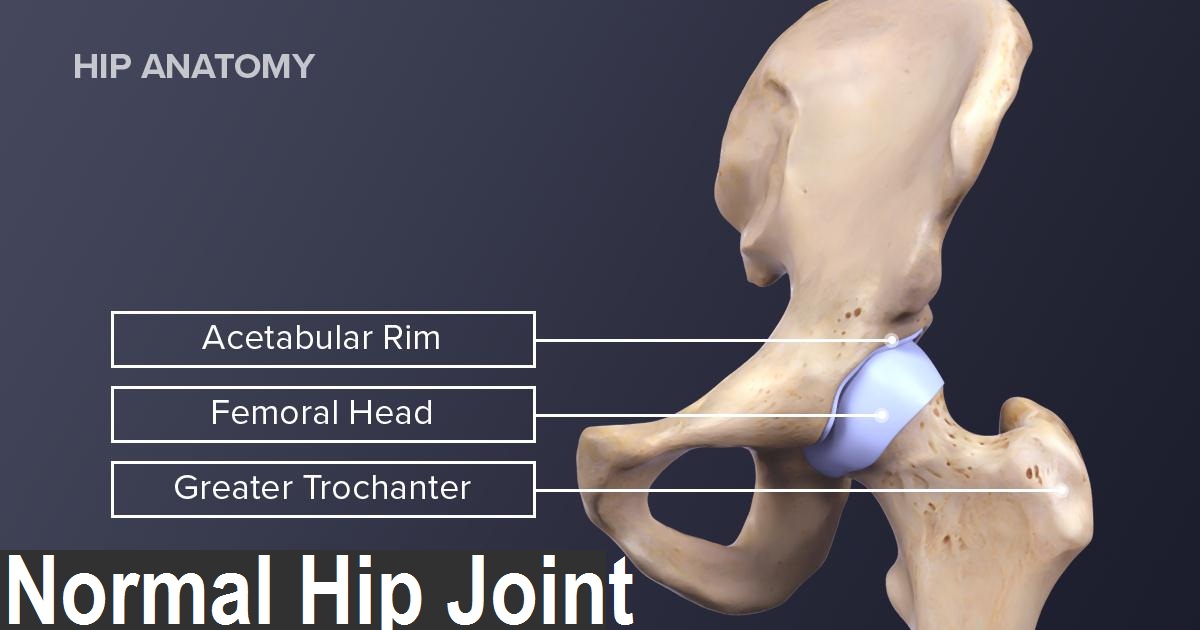
The hip is one of the body's largest joints. It is a "ball-and-socket" joint. The socket is formed by the acetabulum, which is part of the large pelvis bone. The ball is the femoral head, which is the upper end of the femur (thighbone).
The bone surfaces of the ball and socket are covered with articular cartilage, a smooth, slippery substance that protects and cushions the bones and enables them to move easily. The surface of the joint is covered by a thin lining called the synovium. In a healthy hip, the synovium produces a small amount of fluid that lubricates the cartilage and aids in movement.
Description
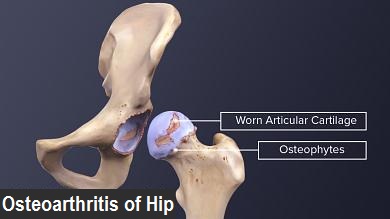
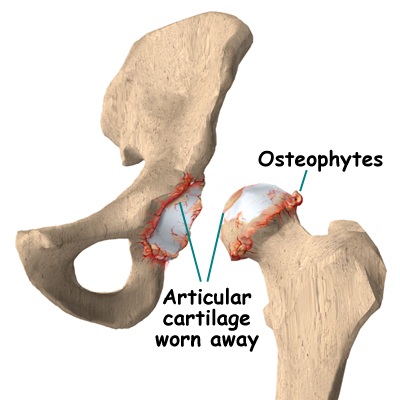
Osteoarthritis is a degenerative type of arthritis that occurs most often in people 50 years of age and older, though it may occur in younger people, too. In osteoarthritis, the cartilage in the hip joint gradually wears away over time. As the cartilage wears away, it becomes frayed and rough, and the protective joint space between the bones decreases. This can result in bone rubbing on bone. To make up for the lost cartilage, the damaged bones may start to grow outward and form bone spurs (osteophytes).
Osteoarthritis develops slowly and the pain it causes worsens over time
Cause
Osteoarthritis has no single specific cause, but there are certain factors that may make you more likely to develop the disease, including:
- Increasing age
- Family history of osteoarthritis
- Previous injury to the hip joint
- Obesity
- Improper formation of the hip joint at birth, a condition known as developmental dysplasia of the hip
Even if you do not have any of the risk factors listed above, you can still develop osteoarthritis.
Symptoms
The most common symptom of hip osteoarthritis is pain around the hip joint. Usually, the pain develops slowly and worsens over time, although sudden onset is also possible. Pain and stiffness may be worse in the morning, or after sitting or resting for a while. Over time, painful symptoms may occur more frequently, including during rest or at night. Additional symptoms may include:
- Pain in your groin or thigh that radiates to your buttocks or your knee
- Pain that flares up with vigorous
- Stiffness in the hip joint that makes it difficult to walk or bend
- "Locking" or "sticking" of the joint, and a grinding noise (crepitus) during movement caused by loose fragments of cartilage and other tissue interfering with the smooth motion of the hip
- Decreased range of motion in the hip that affects the ability to walk and may cause a limp
- Increased joint pain with rainy weather


Examination by Doctor
During your appointment, doctor will talk with you about your symptoms and medical history, conduct a physical examination, and possibly order diagnostic tests, such as x-rays.
Physical Examination

During the physical examination, Doctor will look for:
- Tenderness about the knee
- Range of passive (assisted) and active (self-directed) motion
- Instability of the joint
- Crepitus (a grating sensation inside the joint) with movement
- Pain when weight is placed on the hip
- Pain when pressure is placed on the hip
- Problems with your gait (the way you walk)
- Any signs of injury to the muscles, tendons, and ligaments surrounding the hip
Imaging Tests
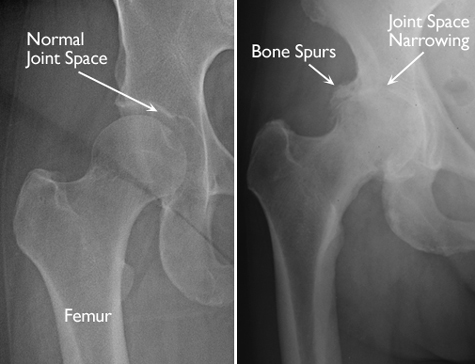
X-rays.- These imaging tests create detailed pictures of dense structures, like bones. They can help distinguish among various forms of arthritis. The plain radiograph serves as the primary investigation in the diagnosis of knee OA, as well as in assessing the severity of the disease. X-rays of an arthritic knee may show a narrowing of the joint space, the formation of bone spurs (osteophytes), changes in the bone like subchondral bone sclerosis & cyst formation, osteochondral bodies and bone deformities.
Treatment
Although there is no cure for osteoarthritis, there are a number of treatment options that will help relieve pain and improve mobility.
(A)Nonsurgical Treatment
As with other arthritic conditions, initial treatment of arthritis of the knee is nonsurgical. Doctor may recommend a range of treatment options.
1.Lifestyle modificationsSome changes in your daily life can protect your knee joint and slow the progress of arthritis.
- Minimize activities that aggravate the condition, such as climbing stairs.
- Switching from high impact activities (like jogging or tennis) to lower impact activities (like swimming or cycling) will put less stress on your knee.
- Losing weight, if you are obese , can reduce stress on the hip joint, resulting in less pain and increased function.
2. Physical therapy Specific exercises can help increase range of motion and flexibility, as well as strengthen the muscles in your hip and leg. Doctor or physical therapist can help develop an individualized exercise program that meets your needs and lifestyle.
3. Assistive devices Using walking supports like a cane, crutches, or a walker can improve mobility and independence. Using assistive aids like a long-handled reacher to pick up low-lying things will help you avoid movements that may cause pain.
3. Medications If your pain affects your daily routine, or is not relieved by other nonsurgical methods, doctor may add medication to your treatment plan.
(B)Surgical Treatment
Doctor may recommend surgery if your pain from arthritis causes disability and is not relieved with nonsurgical treatment.
1. Osteotomy Either the head of the thighbone or the socket is cut and realigned to take pressure off of the hip joint. This procedure is used only rarely to treat osteoarthritis of the hip.
2. Hip resurfacing In this hip replacement procedure, the damaged bone and cartilage in the acetabulum (hip socket) is removed and replaced with a metal shell. The head of the femur, however, is not removed, but instead capped with a smooth metal covering.



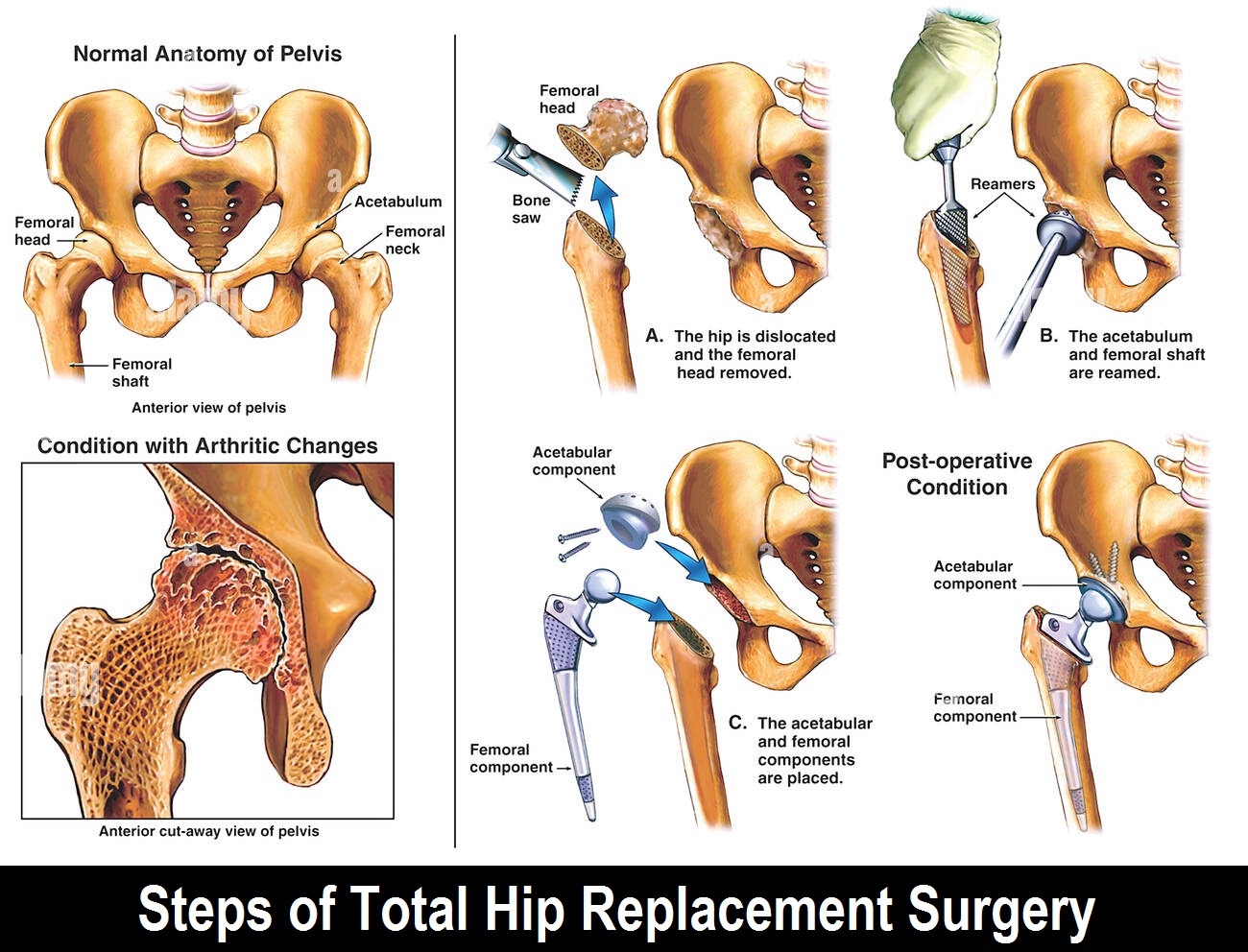
3. Total hip replacement The hip joint is a “ball and socket joint”. It is a very important joint as it allows a great deal of movement but is also weight-bearing. As a result of this, it is often prone to “wearing away”. This is a simplified reason as to why arthritis occurs. Arthritis can be a very painful disorder which may slow down your mobility/ walking or even stop you from sleeping.
A hip replacement is an operation which replaces the severely damaged hip bone with an artificial ball and socket that does the function of the natural joint. It may reduce the pain and help in walking and sleeping.
An anaesthetic will be given in theatres. This may be a general anaesthetic (where you will be asleep) and/ or a regional block (e.g. where you are awake but the area to be operated is completely numbed) for example an injection into the spine. You must discuss this and the risks with the anaesthetist. If you have any allergies, please also tell them.
You will lie on the opposite side to the one being operated on. Your skin will be cleaned with antiseptic fluid and clean towels (drapes) will be wrapped around the hip.
The surgeon will make a cut (incision) using a surgical knife (scalpel). The exact location of the incision depends on your surgeon’s technique. The length of the incision also depends upon the surgeon and your leg.
A cut is made through the fat and muscles which lie in the way of the hip bones. The top of the thigh bone (femur) which forms the neck and ball will be cut away. A replacement stem and ball can then be placed in the remaining thigh bone.
The socket part of the hip joint will also be drilled smooth. The surgeon will try and remove as much arthritic bone and make a smooth base for the new “cup”. In some cases, surgeons will use a special bone cement to hold the stem and/ or the cup in position. There are also different types of materials of implant to use. These can be made of different types of metals, polyethylene (like a plastic) or very tough ceramic / oxinium. When satisfied with the positions, the surgeon will close the wound. A drain may be used. This allows any collections of blood or fluid to drain out. The drain can be removed painlessly on the ward within a day or two. The skin can finally be closed. Some surgeons use stitches, while others prefer metal clips (skin staples). Both methods are equally successful and come down to surgeon preference. When you wake up, you will feel sore around the hip, this is normal. You will be encouraged to start walking as soon as possible with the aid of the physiotherapists. An X-ray and a blood test may be taken the same or next day
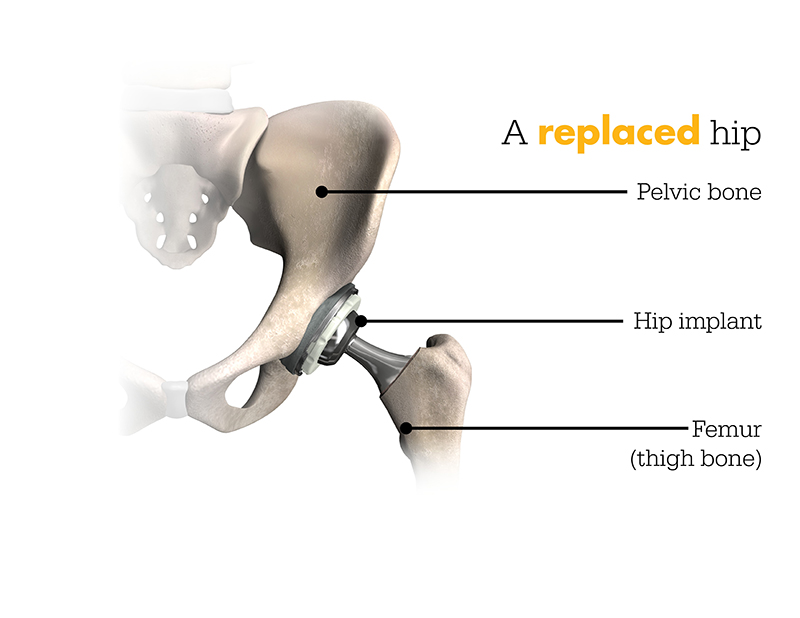
TOTAL HIP REPLACEMENT IMPLANTS

STEPS OF TOTAL HIP REPLACEMENT(THR) SURGERY
Meet Our Doctors

Dr. Nitin Thakkar
M.S (Ortho)

Dr. Shweta Thakkar
DMRD, DNB (Radio-Diagnosis)
